Basic features
The clinical laboratory data of the patients with PBC-CREST are shown in Table 1. The mean age of the 302 PBC patients at diagnosis was 59 years, and the cohort included 49 men and 253 women. Patients with PBC-CREST had significantly lower levels of alanine aminotransferase (ALT), gamma-glutamyl transpeptidase (γ-GTP), and total bilirubin (TB) than patients with PBC only. In patients with PBC-CREST, the prevalence of anti-centromere antibodies (ACA) was higher and the prevalence of AMA positivity was lower than in patients with PBC only. In addition, patients with PBC-CREST had a significantly lower prevalence of cirrhosis than patients with PBC only. Although there was no significant difference in the prevalence of varices between patients with PBC-CREST and patients with PBC alone, the rate of progression to cirrhosis was higher in patients with PBC alone than in patients with PBC-CREST. The median follow-up period was 6.3 years, during which there were 6 liver transplantations (LT) and 37 cases of liver-related death (LRD). Of the 245 patients with PBC alone, 207 received UDCA monotherapy and 34 patients received combination therapy with UDCA and BF. Of the 57 patients with PBC-CREST, 56 received UDCA monotherapy and 1 patient received combination therapy with UDCA and BF (Fig. 1).

Flowchart of the patient selection process.
Analysis of survival after UDCA treatment
The median follow-up time from diagnosis was 6.3 years. The 3/5/10-year LT-free survival rates were 92/87/80% in the PBC alone group and 98/96/96% in the PBC-CREST group, with the prognosis being significantly better in the PBC-CREST group (log-rank P= 0.0172) (Fig. 2).
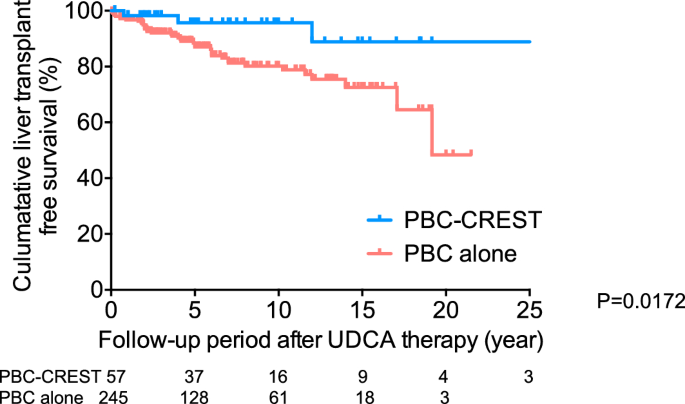
Analysis of survival after UDCA treatment (n = 302). Probability of LT-free survival in 302 patients with PBC calculated using the Kaplan-Meier method. Patients with PBC were classified at baseline as patients with PBC alone (n = 245) or PBC-CREST (n = 57). The rate of LRD or LT was significantly lower in patients with PBC-CREST than in patients with PBC alone (log-rank test).
Univariate and multivariate analysis of risk and protective factors associated with liver-related death or liver transplantation in patients with primary biliary cholangitis
The results of univariate and multivariate Cox proportional hazard regression analyses of risk factors and protective factors significantly associated with LRD/LT are shown in Supplementary Table 1 and Table 2, respectively. Univariate analysis revealed that the following factors were significantly associated with LRD/LT: ACA positivity, the presence of liver cirrhosis (LC), the presence of CREST syndrome, AST > 43 U/L, ALT > 46 U/L, ALP > 499 U/L, TB > 0.97 mg/dL, ALB ≤ 3.6 g/dL, and platelet count (PLT) ≤ 12.8 × 104/μL. Multivariate analysis was performed using the factors identified as significant by univariate analysis. After adjusting for confounding variables such as age, gender, ACA status, LC status, and CREST status, the hazard ratio (HR) for LRD/LT in patients with LC was 20.7 (95% confidence interval (CI) 9.46-45.3). After adjusting for confounding variables such as age, gender, ACA status, LC status, CREST status, AST concentration, ALT concentration, and ALP concentration, the HR for LRD/LT in patients with LC was 17.7 (95% CI 7.71-40.8). After adjusting for confounding variables such as age, gender, ACA status, LC status, CREST status, TB concentration, ALB concentration, and PLT number, the HR for LRD/LT in patients with serum ALB concentration ≤ 3.6 g/dL was 4.16 (95% CI 2.10–8.22) and the HR for LRD/LT in patients with LC was 12.9 (95% CI 5.21–32.1). The presence of LC and serum ALB concentration ≤ 3.6 g/dL were identified as independent factors (P< 0.0001).
Multivariate analysis of factors associated with liver cirrhosis in patients with primary biliary cholangitis
A total of 302 PBC patients were included in the final analysis, of whom 247 had no LC (non-LC patients) and 55 had LC. The baseline characteristics of the patients are shown in Supplementary Table 2. Compared with PBC patients without LC, PBC patients with LC had significantly higher concentrations of AST, ALP, TB, IgG and IgM, and significantly lower ALB concentrations and PLT counts. As expected, the complication rate with CREST syndrome was higher in PBC patients without LC than in patients with LC. Multivariate analysis was performed using the factors identified as significant for LC. After adjusting for confounding variables such as age, gender, AMA status, ACA status and CREST status, the presence of CREST syndrome was found to be an independent protective factor. The odds ratio (OR) for LC with the presence of CREST syndrome was 0.24 (95% CI 0.07–0.83) (Table 3).
Effects of UDCA treatment on liver biochemistry
The clinical laboratory data of the 173 patients with PBC alone or PBC-CREST at baseline, excluding patients with LRD/LT within 12 months of diagnosis and patients who were not evaluable after 12 months of UDCA administration, are presented in Supplementary Table 3. A significantly larger proportion of patients with PBC-CREST than those with PBC alone were female, and they had lower γ-GTP levels. The effects of UDCA therapy on liver biochemistry are shown in Supplementary Figure 1. A comparison of liver biochemistry between patients with PBC alone and patients with PBC-CREST after 12 months of UDCA treatment showed that TB concentration in patients with PBC alone was not significantly decreased after treatment, although ALP and ALT concentrations in patients with PBC alone were significantly decreased after treatment. On the other hand, TB, ALP and ALT concentrations in patients with PBC-CREST were significantly decreased after treatment. Serum ALB concentration and PLT count were not significantly increased after treatment in patients with PBC alone or in patients with PBC-CREST.
Analysis of Globe Scores after UDCA treatment
The results of the comparison of the estimated survival rates, calculated using the GLOBE score, between patients with PBC alone and patients with PBC-CREST are shown in Fig. 3. The mean GLOBE score of patients with PBC alone after UDCA therapy was 0.88 ± 0.93 (range: − 1.01 to 4.60), while the mean GLOBE score of patients with PBC-CREST was comparatively significantly lower (P< 0,05, Mann-Whitney-U-Test) auf 0,47 ± 0,78 (Bereich: − 1,12 bis 2,09) (Abb. 3A). Darüber hinaus hatten 73,5 % bzw. 57,6 % der Patienten mit PBC allein bzw. PBC-CREST einen GLOBE-Score von > 0.3, which is considered to indicate a UDCA non-responder with a significantly shorter LT-free survival time than a comparable healthy patient. In addition, the 3-/5-year LT-free survival rates calculated using the GLOBE score were significantly higher in the PBC-CREST group (93/88%) than in the PBC-alone group (88/81%) after UDCA therapy (P< 0.05) (Fig. 3B,C).
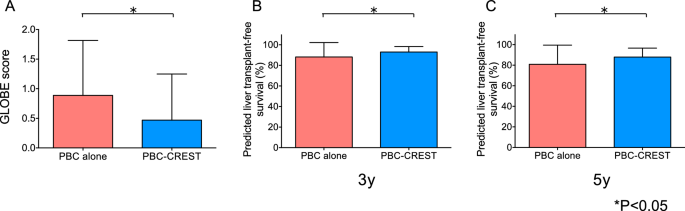
Analysis of the GLOBE score after UDCA treatment (n = 173). The GLOBE scores (A) and forecast 3-year (B) and 5-year (C) LT-free survival rates were calculated for patients with PBC-CREST compared with patients with PBC alone after UDCA treatment. Data are expressed as means ± SEMs and the statistical significance of differences was assessed using the nonparametric Mann-Whitney U test.
Analysis of UK-PBC risk scores after UDCA treatment
The 5/10/15-year risks of LRD or LT were significantly lower, as predicted by the UK-PBC risk score (P< 0.05) in patients with PBC-CREST (2.4/7.6/13.2%) than in patients with PBC alone (4.8/11.8/18.8%) after UDCA therapy (Fig. 4A–C).

Analysis of the UK-PBC risk score after UDCA treatment (n = 173). The predicted risks of LRD or LT after 5 years (A), ten years (B) and 15 years (C) were calculated 12 months after UDCA treatment and compared between patients with PBC-CREST and patients with PBC alone. Data are expressed as means ± SEMs and the statistical significance of differences was assessed using the nonparametric Mann-Whitney U test.




