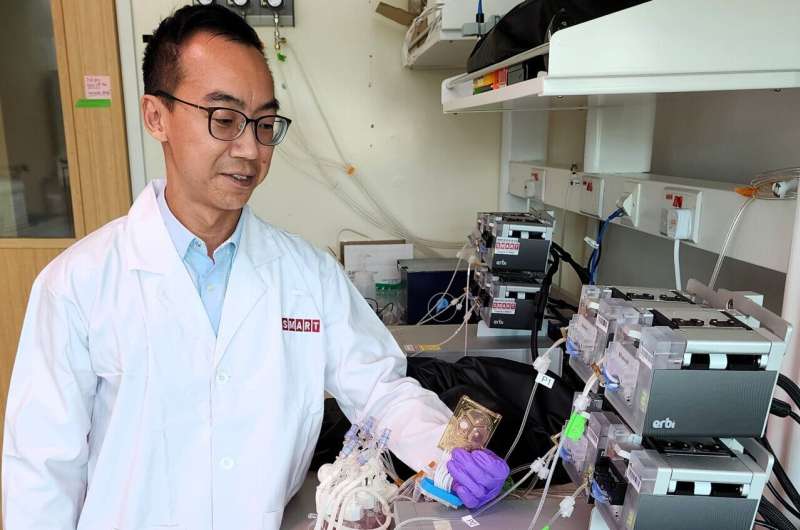
SMART researcher Dr. Wei-Xiang Sin holds the microfluidic chip in which T cells are activated, transduced and expanded in a 2-milliliter growth chamber. Image credit: SMART CAMP
Researchers have developed a novel method to produce viable autologous chimeric antigen receptor T cells (CAR-T cells) at clinical doses in an ultrasmall, automated, closed-system microfluidic chip approximately the size of a deck of cards.
The team from the Critical Analytics for Manufacturing Personalized-Medicine (CAMP) Interdisciplinary Research Group (IRG) at the Singapore-MIT Alliance for Research and Technology (SMART), MIT’s research venture in Singapore, collaborated with researchers from the Duke-NUS Medical School (Duke-NUS), the Institute of Molecular and Cell Biology (IMCB) at the Agency for Science, Technology and Research (A*STAR), the KK Women’s & Children’s Hospital (KKH), and the Singapore General Hospital (SGH).
This method is the first to use a microbioreactor to produce autologous cell therapy products. In particular, the new method has been successfully used to produce and expand CAR-T cells that are as effective as cells produced using existing systems, while requiring less space and equipment, and fewer seed cells and cell production reagents.
This could lead to more efficient and cost-effective methods for scaling up the manufacturing of autologous cell therapies and potentially even enable point-of-care manufacturing of CAR-T cells outside of laboratory settings – for example, in hospitals and wards.
The production of CAR-T cell therapy requires the isolation, activation, genetic modification and expansion of a patient’s own T cells to kill tumor cells when reinfused into the patient.
Despite the revolution that cell therapies have experienced in cancer immunotherapy, with some of the first patients to receive autologous cell therapy achieving remission for more than ten years, the manufacturing process of CAR-T cells remains inconsistent, expensive and time-consuming.
It is prone to contamination, human error, and requires cell numbers that are impractical for smaller-scale production of CAR-T cells. These challenges create bottlenecks that limit both the availability and affordability of these therapies, despite their effectiveness.
In an article entitled “High-density microbioreactor process for automated point-of-care production of CAR-T cells” published in Nature Biomedical EngineeringThe CAMP researchers describe their breakthrough: Primary human T cells can be activated, transduced and proliferated to high densities in an automated, two-milliliter closed-system microfluidic chip to produce over 60 million CAR-T cells from donors with lymphomas and over 200 million CAR-T cells from healthy donors.
CAR-T cells produced in the microbioreactor are as effective as those produced using traditional methods, but require less space and resources. This results in lower manufacturing costs and potentially lower costs for patients.
At high T cell expansion rates, similar total T cell numbers could be achieved with a shorter culture time in the microbioreactor (seven to eight days) compared to gas permeable culture plates (12 days), potentially reducing production times by 30 to 40%.
The researchers showed that the CAR-T cells from the microfluidic bioreactor and the gas-permeable culture plates showed only minor differences in cell quality. When tested on mice, the cells were equally functional in killing leukemia cells.
“This new method suggests that dramatic miniaturization of current-generation autologous cell therapy production is possible, with the potential to significantly reduce the manufacturing limitations of CAR-T cell therapy. Such miniaturization would lay the foundation for point-of-care manufacturing of CAR-T cells and reduce the required ‘good manufacturing practice’ (GMP) footprint for cell therapy manufacturing – which is one of the key drivers of COGM,” said Wei-Xiang Sin, research scientist at SMART CAMP and first author of the paper.
Of particular note is that the microbioreactor used in research is a perfusion-based, automated, closed system with the smallest space requirement per dose, the smallest culture volume and the smallest number of seed cells, as well as the highest achievable cell density and process control.
These microbioreactors – previously used only for microbial and mammalian cell culture – were originally developed at MIT and further developed for commercial production by Millipore Sigma.
The small number of starting cells required compared to existing larger automated manufacturing platforms means that smaller quantities of isolation beads, activation reagents and lentiviral vectors are required per production run.
In addition, due to the extremely small culture volume (2 milliliters; approximately 100 times less than larger automated culture systems), smaller amounts of media are required (at least 10 times less than larger automated culture systems), contributing to a significant reduction in reagent costs. This could benefit patients, particularly pediatric patients, who have low or insufficient T cell numbers to produce therapeutic doses of CAR T cells.
“This advance in cell therapy manufacturing could ultimately provide a point-of-care platform that could significantly increase the number of CAR T cell manufacturing slots, reducing the wait times and production costs of these living drugs – making cell therapy more accessible to the masses,” said Michael Birnbaum, co-lead principal investigator at SMART CAMP, associate professor of bioengineering at MIT, and co-author of the paper.
“The use of smaller bioreactors could also support process optimization studies, including for various cell therapy products.”
In the future, SMART CAMP is working on further developing sampling and/or analysis systems around the microbioreactor so that CAR-T production can be carried out with fewer personnel and outside of a laboratory, potentially facilitating the decentralized production of CAR-T cells at the bedside.
In addition, SMART CAMP aims to further optimize process parameters and culture conditions to improve cell yield and quality for future clinical use.
More information:
Wei-Xiang Sin et al., A high-density microfluidic bioreactor for automated CAR-T cell production, Nature Biomedical Engineering (2024). DOI: 10.1038/s41551-024-01219-1
Provided by Singapore-MIT Alliance for Research and Technology
Quote: Researchers pioneer production of CAR-T cells using high-density microfluidic bioreactor (June 27, 2024), accessed June 27, 2024 from https://medicalxpress.com/news/2024-06-production-car-cells-high-density.html
This document is subject to copyright. Except for the purposes of private study or research, no part of it may be reproduced without written permission. The contents are for information purposes only.